Introduction
The temporomandibular joint (TMJ) connects your mandible in condylar
process (lower jaw) to your skull in mandibular fossa , The joint can be located facing your ears on both sides of your head ,It lets your jaw open and close, helping you to talk and feed.
This abbreviation has also been used to refer to a category of health conditions related to the jaw, although this is becoming more frequently abbreviated as TMD or TMJD in order to differentiate between the temporomandibular joint itself and TMJ, These disorders may cause joint
tenderness, facial pain and difficulty moving the joint.
As many as 10 million Americans suffer from TMJD according to the National Institute of Dental and Craniofacial Studies. TMJD is more common among women compared with men, These diseases may be controlled but there are several potential causes,That can complicate the diagnosis.
The temporomandibular joint (TMJ) or jawjoint is a bi-arthroidal hinge joint that allows for the lifelong complex movements .
Headline
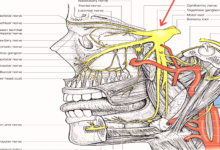
TMJ structures
Capsules And Articular Disc
The capsule is a thick fibrous membrane that encircles the joint and integrates the eminence of the articular,It attaches to the eminence of the articulate, articular disc, and mandibular condyle neck.
The Articular Disc is the distinguishing characteristic of the temporomandibular
joint, The disk consists of dense fibrocartilagenous tissue which is placed between the mandibular condyle head and the temporal bone mandibula fossa, Temporal mandibular joints are one of the few synovial joints with an articular disk in the human body, another being the sternoclavicular joint , The disks split each joint into two compartments, the upper and the lower , These two compartments are synovial cavities which consist of a synovial cavity upper and lower ,The joint capsule lining synovial membrane creates the synovial fluid that fills those cavit (1) .
The central area of the disk is avascular and lacks innervation, thus deriving its
nutrients from the synovial fluid surrounding it, In contrast, it has both blood vessels and nerves along the posterior ligament and the surrounding capsules, There are few cells but among them are fibroblasts and white blood cells, The central area is also thinner but more dense than the peripheral region, It is thicker but contains more cushioned.
The synovial fluid in the synovial cavities provides nutrients for the central avascular region of the disk , With age, the entire disc thins, and may undergo cartilage addition in the central part, changes that may result in impaired joint movement Except for the surface of the articular disc and condylar cartilage, the synovial membrane covers the inner surface of the articular
capsule within the TMJ (2) .
The lower joint compartment formed by the mandible and the articular disk is
involved in rotational motion ,this is the jaw’s initial motion when the mouth is
opened, Translational movement involves the upper joint compartment formed by the articular disk and the temporal bone, this is the jaw ‘s secondary gliding motion as it is widely opened ,The part of the mandible that mates to the underside of the disk is the condyle , and the part of the temporal bone that mates to the upper surface of the disk is the articular fossa or fossa of glenoid or mandibular, The articular disk is a fibrous part of the capsule in between the joint’s two bones , The disk acts as articular surfaces against both the temporal bone and the condyles and, as already mentioned, divides the joint into two parts,This is biconcave in shape, and medially and laterally binds to the condyle ,The anterior portion of the disc splits in the vertical dimension, which corresponds with the insertion of the lateral pterygoid’s superior ear.
The subsequent portion also splits in the vertical dimension, and the area between the split continues later
and is called the retrodiscal tissue, Unlike the disk itself, this piece of connective
tissue is vascular and innervated, and the pain felt during the movement of the
mandible is due to the condyle compressing this area against the temporal bone articular surface in some cases of anterior disc displacement (3).
Ligaments
The temporomandibular joints are connected with three ligaments,
one major, and two minor ligaments, These ligaments are important in defining the boundary movements of the mandible, or in other words, the farthest extent of movements, Movements of the mandible made past the extent that the muscle attachments functionally allow will result in painful stimuli, Therefore, movement outside these more narrow boundaries is rarely accomplished in normal operation, The ligaments give the TMJ a passive stability.
The temporomandibular ligament is the capsule’s thickened lateral portion, and it
has two parts, an external oblique portion, and an internal horizontal portion, The base of this triangular ligament is connected to the temporal bone and articular tubercle zygomatic process; its apex is fixed to the lateral side of the mandibular neck, This ligament prevents the excessive retraction or backward movement of
the mandible, a situation which could lead to joint problems (4) .
The stylomandibular ligament originates from the styloid process and is attached to the angle of the mandible.
It is responsible for allowing a protrude of the mandible.
The sphenomandibular ligament is extended between the spine of the
sphenoid bone and the mandible lingual, This helps reduce the severe protrusive
motions and the opening of the jaws(5)
IN ADDITION TO The oto-mandibular
ligaments are the discomalleolar ligament (DML), which originates from the malleus (one of the middle ear ossicles) and runs through the sphenomandibular ligament to the medial retrodiscal tissue of the TMJ, and the anterior malleolar
ligament (AML)(6).
More explanation in next article
references
1-Fehrenbach M, Popowics T. Illustrated dental embryology, histology, and
anatomy
2-Nozawa-Inoue K, Amizuka N, Ikeda N, Suzuki A, Kawano Y, Maeda T. Synovial membrane in the temporomandibular joint-Its morphology, function and development. Archives of Histology and Cytology. 2003;66(4):289-306.
3- Norton N, Netter F. Netter’s head and neck anatomy for dentistry.
Philadelphia, PA: Elsevier/Saunders; 2012.
4-Temporomandibular joint [Internet]. Kenhub. 2020 [cited 28 May 2020].
Available from: https://www.kenhub.com/en/library/anatomy/the- temporomandibular-joint
5- The Temporomandibular Joint – Structure – Function – TeachMeAnatomy
[Internet]. Teachmeanatomy.info. 2020 [cited 28 May 2020]. Available from:
https://teachmeanatomy.info/head/joints/temporomandibular/
6-Rodriguez Vazquez J, Velasco M, Jimenez Collado J. Relationships between
the Temporomandibular Joint and the Middle Ear in Human Fetuses. Journal of
Dental Research. 1993;72(1):62-66.